Leading Product Edition 1
Introducing Leading Product | Electronic Medical Records | Found Online & In Scholarship | JTBD | Contemplation | Sign Off = 12 minutes.
🌊 Welcome
Welcome to Lead(ing) Product, my new newsletter. Chances are, you’re checking out the archive. I appreciate it. So why am I writing LP? There aren’t enough newsletters about product management. Just kidding. The actual reason: I needed a place to refine some ideas that take up space in my head. Having them down as pixels is a bit of an outlet. Also, I really wanted to share them and get feedback. So here we are.
I’m learning, you’re learning, so we’re learning together and that’s pretty cool.
This edition of LP explores Electronic Medical Record (EMR) software as a product that each of us interacts with, even if we’re not the intended end users. Our health care providers are, and they tend not to exactly love their EMR systems. Sometimes referred to as Electronic Patient (or Health) Records, they aren’t often associated with feelings of delight. Admittedly, this is Western-centric. I’m really curious about experiences with EMR outside of North America.
Then, I’ll highlight recent posts and scholarship of interest, as well as break down an important element from a recent job posting. Each edition, I’ll leave you with something to contemplate (and maybe circle back to attempt an answer in the future).
👩🏽⚕️ Electronic Medical Records enrich my life said no doctor ever
For the first long form article, I had the chance to speak with a few physicians about EMR, which have existed in some form or another since the late 1960s. Ask a physician for an opinion about today’s EMR systems, and they’ll typically say one of two things: either bad, or not great. Not one (in my non-scientific survey) was delighted.
EMRs are used by healthcare providers to digitize aspects of care delivery. Today, there are many EMR providers and the space has undergone a fair bit of consolidation, a trend expected to accelerate. An accurate and accessible EMR is critical to a patient’s care and outcome, since providers use it to document histories and plan treatment protocols, including prescriptions and test results. Adoption varies a lot… and apparently there’s such a thing as too much EMR? According to Tom Sullivan, “Most hospitals have at least 10 EHRs in place and only two percent are down to just a pair of platforms.” Yikes.
Over the course of their life, a person may engage with different health providers (across many networks) and undergo numerous treatments. They may suffer from one medical condition, or many. An illness can be chronic, or acute. An EMR must be flexible enough to allow a healthcare provider to deal with what ails us. That’s tough when a lot ails the EMR. As a complex, transactional system that relies on a lot of human input, today’s EMR solutions are not up for the task: the interfaces are complex, the business logic is way too rigid, they don’t interoperate (due to highly proprietary data structures), etc.
WHY? Is it regulation? Is it because the buyer is often very different and potentially far removed from the end user? Those are likely partial explanations. The myriad of issues has led to poor uptake* and physicians often feel forced to use a hospital’s EMR as a burdensome aspect of their jobs, rather than something that makes it easier to make and keep people well. Paper hasn’t gone away: some records are required to be printed and placed on the patient’s chart, so hybrid records tend to be the norm in a clinical setting.
I’ve condensed and aggregated the opinions shared by different physicians about their use of EMR systems. Yes, it’s anecdotal, but I think it represents a broader consensus about how frustrating some of these products are.
On order sets
We have order sets for common treatment protocols that are normally a combination of activities or consumable items. Setting these up is difficult, and to renew or implement a new order set can be extremely frustrating; I’ve found a workaround, but it’s not obvious to a new physician. Something that is straightforward in real life may be very challenging to input into an EMR. Imagine a new resident at 3 AM trying to request a new order set.
On prescribing medication
I can’t easily start a drug on the same day I see a patient as part of a regime; our EMR requires a dose for the day, and a separate order for the regime going forward. There are challenges with recurring drug regimes, especially those that might have an unconventional schedule, like every other day. Regimes are normally standing or as needed, and the EMR we use requires us to justify the selection at every step. This isn’t a bad thing, but it means I need to scroll through about ten drop down menus trapped in a small window. It’s easy to miss something and it’s so rigid that I often need to restart the entire order flow if there’s an error.
On contra-indications
I get warnings (about drug collisions) all the time, but they make no sense in terms of the treatment I’m ordering. I’ll consult with a different database of collisions to make sure there are no adverse outcomes. The EMR doesn’t do that for me. Furthermore, the EMR can’t accommodate complex medication regimes, like those used in oncology.
On testing
Test results are available in the EMR if the patient has it done in our network, and not an external lab, for example. So I tell my patients to get the test done at the hospital so the results are available digitally.
On patient access
Increasingly, patients have access to their EMR. In general, it’s a good thing. But it’s complicated. In specialties where physicians are trying to document complex histories, relevant to a diagnosis, patients might be exposed to nomenclature without the context that we get from our training and experience. I don’t want to sound paternalistic; physician records are for physicians and notes are a clinic tool that requires context. For example, I had a colleague use the acronym for Bipolar Affective Disorder (BAD) to describe a patient’s condition; the patient didn’t like that and we can appreciate that there’s a negative connotation when “BAD” is ascribed to someone, regardless of their familiarity with professional terminology.
On encounters (of the clinical kind)
Patient encounters are an important dimension that are not well reflected in the EMR; it can be a documentation nightmare for patients receiving care by two or more clinics. It’s way too easy to document under the wrong encounter, since it’s not intuitive or clearly indicated in the system. An encounter type is really more of a medical-legal term and has very little clinical application, since we review notes in chronological order across encounters. If a lawyer requests all the notes from a given encounter, you don’t want to see notes from a completely different provider that could only cause confusion.
The Way Forward
Complaints about EMR are not new. They’re abundant, because I suspect that only a few providers are actually listening to users (i.e. the pharmacists, nurses, doctors, and many other roles that make up the healthcare provider ecosystem). What can EHR companies do to gain an edge in a saturated marketplace, and actually empower patients and their providers alike? These are quick takes, not fully formed ideas:
Make it a platform. Platforms are powerful. They allow developers to build applications on top and across them while ensuring things like compatible protocols, security, etc. Reframe the EMR ‘system’ as a platform on which developers can securely build flexible, specialty-based applications that also leverage a common data tier.
AI-enabled contextual knowledge. There are many documented use cases for AI in medicine. Radiology has been written about extensively. AI-enabled EMR could allow physicians to prescribe complex medication regimes with a helper in the background, looking for contra-indication and recommending altered regimes that have been shown to result in better patient outcomes.
Unleash the data. Drive better patient outcomes by allowing researchers to access the data inside EMRs. Structure it and make it easy to securely transfer to authorized users who can leverage it in large n studies.
Automate the patient facing view. Patient access is important as the person to whom the record pertains can often spot errors and share information accurately with other providers. It's important to have a patient-centric view of the information a healthcare provider would input. Perhaps an automated patient summary, free from acronyms, will give patients greater confidence in their providers and the technology they deploy.
There are so many more takeaways from the interviews. What did you think?
Further (user-centric) reading
Six Stages Of Health Tech Grief Pt. 1 by Nikhil Krishnan (2020) > Out of Pocket is a great newsletter about US healthcare.
It’s Time for a New Kind of Electronic Health Record by John Glasser
🧙🏻 Found Online
How do you think of yourself, in a D&D kind of way? Are product managers warriors or wizards? Dr. Bruce Cameron (MIT’s System Architecture Group) and his team at TSP look into that.
…We found that the more senior PMs tended to spend more time setting a Vision. This trend held up across Tech and Non-Tech, and across company sizes. Rather than see this as correlation ('the more senior you get, the greater your scope of responsibilities'), we believe this is core learning on the role of the PM : the PM has to build a Vision (and sometimes an ecosystem around it).
I’m a huge fan of Bruce’s and was happy to engage on his LinkedIn post about the study:
…Certainly a PM's focus is divided across tactical (the sprint), operational (quarter / epic), and strategic (the roadmap and ecosystem, market positioning) dimensions. I think wizards tend to be the portfolio owners and delegate the hands-on warrior aspects to others to maintain focus while extending coverage. Each needs to be engaged with end users, likely about different things. Outcome would be a really crisp, prioritized roadmap.
Hopefully? What do you think? I went on to share my graphic depicting the “cone” of roadmap clarity:
📚 Found in Scholarship
Academic journals - especially open access ones - are great resources for industry or user research. Each edition I’ll highlight an article of interest, usually one that’s openly available and not behind a 💰🧱 (something else I’ll explore down the road).
Lanzolla, Pesce, and Tucci investigate how firms perform knowledge integration that leads to market adaptability through innovation. It’s a dense meta-analysis. For larger organizations, the framework has a lot of potential to help leaders understand how to learn, and adapt - and recognize the unintended consequences of doing so. They look at a broad set of literature about search, recombination, and digitization to investigate the organizational precursors and their link to “important idiosyncratic tensions.”
What tensions, you ask? 🥊
Digitalization reinforcing vs. overturning existing knowledge structures;
Digitalization substituting vs. complementing existing competences; and,
Digitalization increasing vs. decreasing cognitive and emotional “costs.”
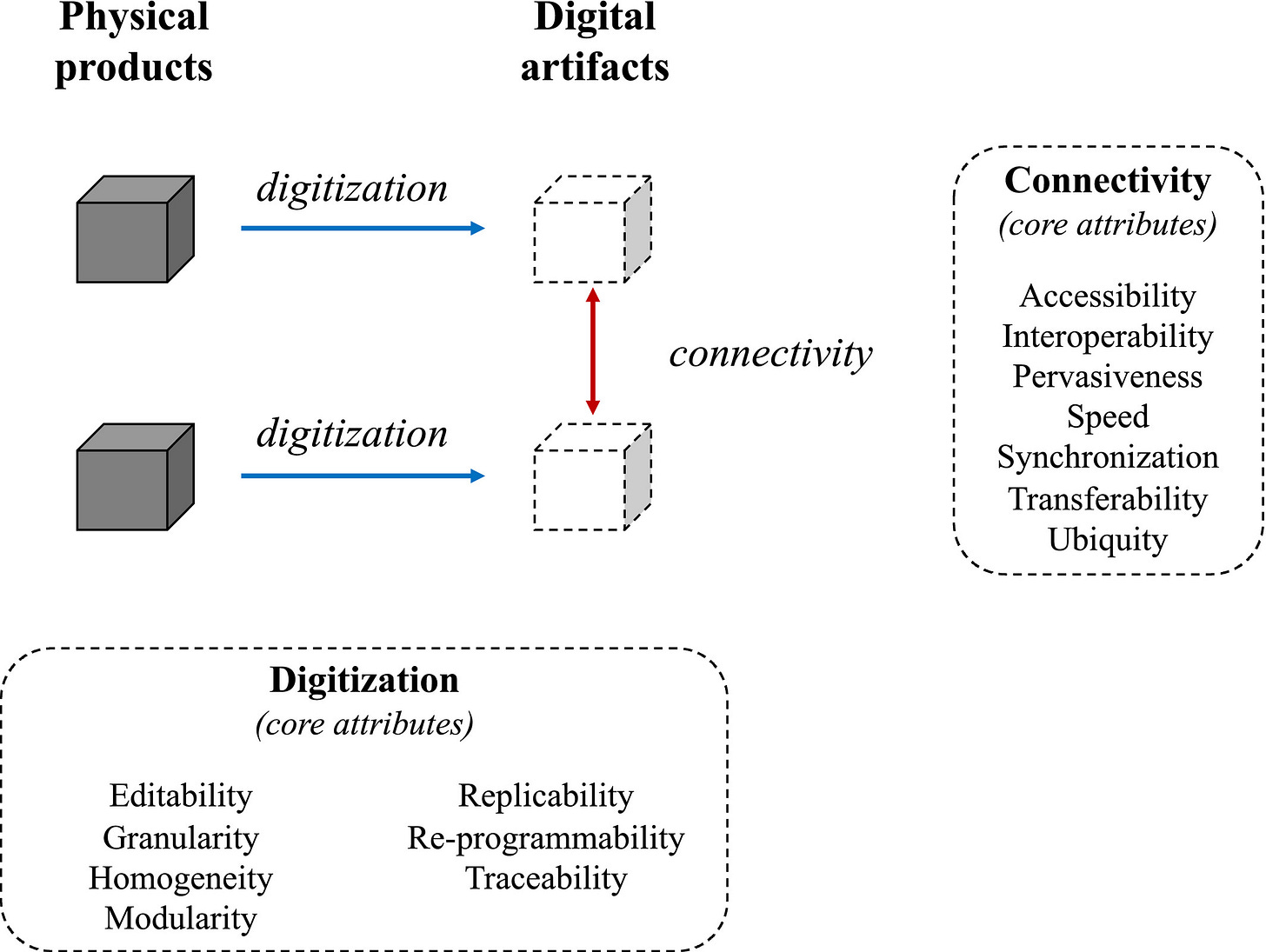
Digitization, to the authors, means moving from a physical product to digital artifact, and which then exhibit a whole bunch of attributes, as well as enable new connections between them. (Digitization can also mean building artifacts for which there is no physical antecedent). They distill a list of properties drawn from across the surveyed literature.
The kicker is that such a transformation can result in whole new ways of thinking and ‘searching’, while it also ups the level of complexity. There are costs (e.g. cognitive load) that come with harnessing or creating digital tooling. Digitization can eliminate silos; paradoxically, it can also inhibit knowledge exchange. One study the authors cite considers that intranet adoption “helped to reinforce the existing functional and national boundaries with ‘electronic fences’ in one firm.” Weird, right?! 😅
There are inherent tensions that accompany any type of transformation. How can leaders (you!) ensure that legacy knowledge structures are pǝuɹnʇɹǝʌo and that people are able stretch “their normal knowledge boundaries” as a result of a digital transformation? Read on for the article’s implications and important lessons for innovation management.
🪛 A Product Job Post - JTBD
PM job advertisements are a wealth of knowledge as well, whether you’re actively searching or not. They show which product management skills are in demand. Each edition I’ll take an element from a job posting and write about it.
“Are you empathetic?"
A recent job advertisement for a senior product manager seeks candidates who can employ the “Job to be Done” approach. Popularized (discovered?) by Clayton Christensen, JTBD is a framework that allows product practitioners to understand how a product fits into a customer’s life; jobs “arise at different points in time and space,” says Christensen. A person wants to do something - have dinner with friends, quickly get breakfast on the way to work (😷), or grow their newsletter subscribers - and your product might enable them to accomplish that thing in a way that was not previously possible or easy.
A prospective customer might not express a need in terms of a feature; rather, they might talk about the course of their day and the challenges they encounter trying to go about it. JTBD helps to break down the key elements that can be mapped to a prospective customer’s or cohort's underlying motivations which, in turn, can be translated to features. It pairs really well with user journey mapping, which should include a view of users’ emotional states (😀😐😔) at different points in a journey through some activity (e.g. taking and posting a photo, finding a dog walker, or ordering dinner). JTBD is an approach, while the user journey map is a visual representation, and both consider a user’s interaction with their surroundings, and the friction points therein.
🎧 Clayton Christensen, who passed away in January 2020, explains it best of course. The HBR IdeaCast podcast re-airs an interview with him in this fantastic episode.
As product managers, we need to engage in high level thinking that is several layers above and below the product itself. JTBD is one framework that provides that kind of perspective.
Contemplation
How does a new feature alter the user’s interaction with existing features? Is the filter more important than the ability to take a great photo in the first place?
Signing Off
That does it for the first edition of Leading Product. Thank you for reading and for sharing! 🙏🏽



